In recent years, LASIK has become one of the commonest operations performed. Its popularity and success are understandable, given the good outcomes experienced by the majority of patients. Still, there are potential side effects with any procedure, and LASIK also has its limitations especially for those with very high spectacle degrees. 2 commonly mentioned alternatives are epiLASIK and ICL (implantable collamer lens), and in Singapore these 2 procedures have been marketed quite heavily as well. Some of their proponents would have you consider undergoing these ops rather than LASIK, and in their reading material sometimes emphasise the potential side effects of LASIK. So, what's the deal with these alternatives and are they really to be preferred over LASIK?
There are pros and
cons with each procedure. With epiLASIK, the advantage (which is also a disadvantage, as you will see later) is that no corneal
flap is created, so theoretically the eye is stronger and perhaps at somewhat
lower risk for a complication called corneal ectasia.
Having said that, the
vast majority of cases that we do are LASIK rather than epiLASIK. Visual
recovery following LASIK is much faster than after epiLASIK. In comparison,
vision the second day after LASIK is already pretty good (usually in the region of 6/6 and 6/7.5), but for epiLASIK, to
reach a comparable level of vision you might need to wait several weeks. We
also take precautions not to go below 250 microns of residual stromal thickness
and this avoids ectasia in normal LASIK patients (the risk being in the
region of 1 in 5000 cases or so).
The problem with
epiLASIK/LASEK/PRK procedures is that the corneal epithelium is removed (see below).
Healing of this to provide a smooth surface will take from several weeks up to
a couple of months or so. Because the surface is ablated, there is a chance of
corneal scarring, but this is much less nowadays since we use mitomycin C at
the end of epiLASIK/LASEK/PRK.
I have grouped
epiLASIK/LASEK/PRK together since they are essentially the same
procedure. The difference is in how the epithelium is removed. In
epiLASIK, a special blunt blade (tissue separator/microkeratome) cleaves the epithelium from the
stroma. There is a risk that the blade may cut into the corneal stroma
sometimes, resulting in an uneven surface, and because of this risk we don't do epiLASIK in our
clinic. LASEK uses alcohol to loosen the epithelium, and this is our method of
choice if we decide on surface treatment for a particular patient. The LASEK we do is 'epithelium-off', or 'alcohol assisted PRK' (see below in italics). Traditional PRK used a
toothbrush type scrubber and we think the alcohol is gentler to the eye. In our clinic we
currently reserve LASEK for patients with corneas that are too thin for
conventional LASIK. The number of patients who have this done is probably less
than 5%. The others all have LASIK with a 'bladeless' technique ie. using
a femtosecond laser to create the flap and then the excimer laser to reshape
the cornea.
A little bit of history: Why, might you ask, did people invent different ways to remove the epithelium when it could very easily be rubbed off with any instrument at hand? Well, it turns out that once people realised how long an eye took to recover from PRK, they tried to keep the thin epithelial cell layer intact and replace it at the end of the operation rather than throwing it away. The 2 ways of separating the epithelium while keeping it intact were 1) using alcohol to loosen the epithelium (LASEK) and 2) using a special blunt blade (epiLASIK). It turns out that once the epithelium is peeled away, whether by alcohol or the blunt blade, it dies. If this dead layer of cells is replaced, it slows healing down even more! Therefore, nowadays, usually even when LASEK or epiLASIK is done the epithelium is thrown away rather than replaced. So that makes it identical to PRK, doesn't it? Why spend money on an epiLASIK blunt blade when you can simply peel away the epithelium, perhaps with alcohol to loosen it first? There just doesn't seem to be a role for epiLASIK...and furthermore when you use a blade, even a blunt one, you run the risk of cutting into the stroma when you don't want to...
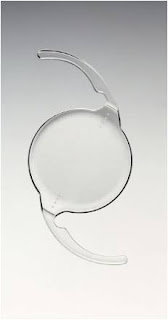
The ICL (above) is similarly different, with different pros and cons. When LASIK is done for patients with very high spectacle degrees or thin corneas, the area of cornea treated (optical zone) is smaller, so that the cornea does not get too thin. Unfortunately, when the area treated is small, the risk of halos in the dark and poorer quality vision also rises. The good thing about the ICL is that halos, even if present, are usually very mild even when the spectacle power corrected is high. It is also true that after ICL, the eye does not get as dry as after LASIK.A little bit of history: Why, might you ask, did people invent different ways to remove the epithelium when it could very easily be rubbed off with any instrument at hand? Well, it turns out that once people realised how long an eye took to recover from PRK, they tried to keep the thin epithelial cell layer intact and replace it at the end of the operation rather than throwing it away. The 2 ways of separating the epithelium while keeping it intact were 1) using alcohol to loosen the epithelium (LASEK) and 2) using a special blunt blade (epiLASIK). It turns out that once the epithelium is peeled away, whether by alcohol or the blunt blade, it dies. If this dead layer of cells is replaced, it slows healing down even more! Therefore, nowadays, usually even when LASEK or epiLASIK is done the epithelium is thrown away rather than replaced. So that makes it identical to PRK, doesn't it? Why spend money on an epiLASIK blunt blade when you can simply peel away the epithelium, perhaps with alcohol to loosen it first? There just doesn't seem to be a role for epiLASIK...and furthermore when you use a blade, even a blunt one, you run the risk of cutting into the stroma when you don't want to...
However, potential intraocular (inside the eye) complications exist with the ICL, of which cataracts and glaucoma are the 2 main (but rare) ones. The main thing about reducing complications with the ICL is to achieve accurate sizing, and at our clinic we do 'sulcus to sulcus' measurements for all ICL patients. What is the sulcus? This is the little nook in the eye just behind the iris (coloured part of the eye) and in front of the original crystalline lens where the ICL will sit. If the ICL is too big for this space in a particular eye, it will be 'squashed', bend forwards, and narrow the drainage angle of the eye (increasing the risk of glaucoma). If the ICL is too small for this space, it will sink backwards and touch the crystalline lens, thus causing a cataract. Although there is no perfect way to measure this sulcus diameter down to the last micron, we have found the Artemis VHF ultrasound biomicroscope (above) to be very accurate and allows us to choose an appropriate size ICL. The figure below shows a measurement made by the Artemis.
I would say that for my patients with lower spectacle
powers, LASIK provides excellent clarity of vision including night vision
(and without the risk of any intraocular complications). I have performed ICL surgery for a number of patients with
excellent results, but I think bearing in mind the potential seriousness of
problems with the ICL my preference is still an extraocular (outside the eye) procedure like LASIK in cases where I judge that the outcome will be
good. Extraocular means zero chance of causing cataract or glaucoma.
Actually, I think the ICL is wonderful, but I prefer to use it for patients with very high powers or
thin corneas, where I feel that the risks of intraocular problems are
outweighed by the better visual quality that can be obtained with the ICL in such cases compared with LASIK.
Although a lens is implanted into the eye in both ICL as well as cataract surgery, an ICL op is quite different from a cataract op, not
least because when an ICL is implanted the patient's original crystalline
lens/cataract is left alone while during a cataract op the crystalline
lens/cataract is removed and is replaced by an intraocular lens implant (IOL). This has implications because there are some doctors out there who perform 'clear lens extractions' to correct high spectacle degrees. If a 'clear lens extraction' (which is like a cataract operation) is done in a younger person less than 45 years old or so, then they will immediately lose the ability to focus for near ie develop immediately the maximum amount of presbyopia/LaoHua. ICL surgery will not affect the development of presbyopia, nor can it cure this problem. ICL surgeons can offer monovision with the ICL, just like with LASIK or contact lenses.
On the other hand, if somebody has a
cataract then he/she should have a cataract op, not an ICL op. The ICL surgery
doesn't do anything about a cataract, which would continue to blur the
vision.
Overall I would say, go for LASIK if your cornea is thick enough because the theoretical advantages of epiLASIK probably do not bear out clinically for the majority of patients. ICL surgery is a great option for those who would otherwise be at risk for visual or other side effects from LASIK.
|














.JPG)