A middle aged man was on his way to Bangkok from Singapore when he felt something blow into his eye at the airport. Trying to clear the irritation, he rubbed his eyes. The irritation persisted and while in Bangkok a doctor could not find anything wrong and patched the eye up. Unfortunately, this did not help much.
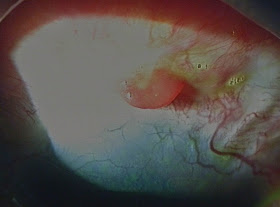
He returned to Singapore the next day at the end of the work trip and when I saw him the eye was obviously red and tearing. The picture below shows a green area with surrounding green dots and lines. These represent raw areas on the surface of the eye where the surface cells (epithelium) have been scratched away.
(Note: I have put some fluorescein drops into the eye-this vegetable based dye tends to stick to raw areas, and gives off a green light when blue light is shone onto it. This makes it very valuable for highlighting abrasions/scratches ont he eye. )
Even before I did anything else, I knew there was something still in the eye. The green lines indicated that very fresh scratches were occurring at the time itself by blinking and eye movements. I automatically 'everted' the eyelid (turned it so that the inner surface faces outwards-some small children like my youngest daughter can do it as a trick to look like a ghoul [below]!)
The picture below shows a tiny yellow spot just to the left of center. The yellowness is actually from the fluorescein dye-if I had not put fluorescein in, it would have been invisible as it was transparent.
Having found the culprit, it was a simple thing to get a pair of jeweller's forceps (mini tweezers) to grab and remove the foreign body. Most of the time when we remove such things, it is impossible to say what it was or where it came from. The picture below shows the offending object at the end of the forceps-a nondescript, fluorescein stained stiff strand-I suspect some little bit of plastic.
When looking for such things, I am fortunate enough to have a slit lamp microscope and of course, the good ol' fluorescein. Very few things escape such scrutiny. Except...
There was a similar case that initially flummoxed me a couple of years ago. A Japanese lady went to the Accident and Emergency Department of a local hospital and I was called to see her. She similarly complained of a stubborn, persisting scratchy sensation in her eye. I did my usual, but try as I might, I could not see a foreign body. She certainly did have scratches on the cornea, but with no sign of a foreign body even with fluorescein eyedrops instilled, I thought the foreign body had been washed out by her tears. I inserted a bandage contact lens and she felt better.
I checked on her a couple of days later and she said she was feeling fine, so I removed the bandage contact lens. Almost immediately, she started tearing and as I looked, scratches were starting to appear on the cornea again! (See pic below) So I everted the eyelid at the slit lamp, but still could not see anything. OK, this calls for plan B...
I brought her to our small treatment room and used an operating microscope this time. With her lying down I could 'double evert' the eyelid-lo and behold-there was a small stitch protruding from the inner surface of the upper eyelid!
NB: In double eversion we evert the eyelid a second time to expose things even higher up in the little pocket called the 'conjunctival fornix'. This stitch was at the upper end of the stiff 'skeleton' of the eyelid, the tarsus.
It turned out that she had double eyelid surgery some years ago, and the person doing it had used a method utilising just stitches. These stitches are often permanent, and do not dissolve on their own. Over time, it had slowly eroded out through the inner surface of the eyelid and the ends of the stitch were now poking the cornea. With that, it was a simple matter to cut the stitch and remove it-problem solved.
Did the double eyelid disappear? No, because after some months collagenous 'scar' tissue forms around the stitch and anchors the skin around the eyelid fold down to the underlying tissues, thus creating a permanent effect that persists even if the stitch is taken out.
I guess the message is, if there is any stubborn grit/irritation in the eye, firstly don't rub the eye, and secondly don't hesitate to visit your friendly eye doctor!