Mr C is an old patient of mine. I first met him 3 years ago, soon after moving to Singapore from Penang.
His is a story of survival, of successfully battling leukemia and unfortunately then losing vision in one eye from complications of graft vs host disease. At the time of his leukemia treatment, he was fortunate enough to receive a bone marrow transplant from one of his sisters, and he subsequently went into remission. The bone marrow unfortunately produced cells which started attacking parts of his body. Some scarring developed in his mouth, but it was his right eye which bore the brunt of it. Treatment with high doses of steroids produced steroid induced glaucoma in the eye, for which he underwent transscleral cyclodiode laser treatment. Unfortunately, that eye became phthisical.
When I first met him, he was just starting to develop inflammation in his other eye. We managed to control that with oral steroids at the beginning, but soon a tongue of fibrovascular tissue started growing inexorably towards the centre of his cornea from under his upper eyelid.
We got him a haematology referral, put him on other immunosuppressants, searched the literature for graft vs host disease, and got nowhere. His vision was soon obscured by the fibrovascular ingrowth. At first, I did a simple excision of this tissue, but ominously it grew back within a matter of months.
I had read reports of oral mucosal transplantation to the ocular surface, but had up to this time been somewhat skeptical of the reported benefits. For this patient, there were not many alternatives. The superior fibrovascular tissue had obliterated the superior conjunctival fornix, and at a minimum I would need some tissue to resurface that. There was no significant tissue to take from his other, phthisical eye. I got my plastic surgeon brother and together we worked on Mr C. He harvested a rectangle of oral mucosa, following which I dissected Mr C's upper lid free of the cornea. I then transplanted the oral mucosa to the uppermost part of the tarsal surface of the upper lid. The surface of the eyeball I covered with a layer of amniotic membrane.
It was with dismay that I noticed fibrovascular tissue creeping across the amniotic membrane a few weeks after surgery. Before long we would be back to square one!
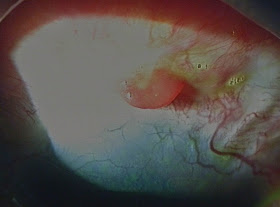
I took Mr C to the treatment room, and slightly out of desperation took a very thin layer (split thickness, see pic below) of the transplanted oral mucosa from the superior forniceal area and retransplanted this to his superior limbal area, hoping that this would act as a barrier to further fibrovascular ingrowth. Amazingly, it did just that! The fibrous tissue regressed into a small red granuloma (see below), which I easily excised in clinic. Epithelium from the oral mucosa in the limbal area also started growing over the cornea, which was soon epithelialised. Amazing, and here we are with so much research done trying to grow oral mucosal epithelium in the lab.
And we all live happily forever after? Unfortunately, no.
After about a year, it became apparent that things were still unstable. Firstly, blood vessels started growing into the superior part of the cornea (see below). Obviously, the oral mucosal cells do nothing to stop blood vessels from growing in. Anytime I tried to reduce his oral steroids and immunosuppression, his conjunctiva and even cornea would get inflamed, with epithelial defects and even more alarmingly, slowly progressive corneal thinning. Secondly, his long term usage of oral steroids had caused a very dense posterior subcapsular cataract. We got by, by keeping him dilated with atropine so he could still see out of the less affected peripheral lens.
But we knew that things were not getting any better. And I was worried that one day his cornea would melt and perforate (as has happened to one of my Stevens Johnson patients before). What he really needed was limbal stem cells that were immune to attack from the transplanted bone marrow. A light bulb went off-I would use limbal tissue from the sister who had donated the bone marrow in the first place! As the immune cells and the limbal tissue are from the same donor, the limbal tissue would naturally be immune from attack!
We discussed this a number of times, and finally about a month ago I sat down and spoke to quite a few of the siblings (they are a large family). As expected, the sister involved wanted to know how the limbal stem cell harvest would affect her. I replied that it was a very safe procedure that would cause very temporary and mild discomfort, although it could cause some changes in spectacle power/astigmatism.
Last week I performed the operation to remove the cataract as well as transplant the limbal stem cells from the sister to Mr C. Both are doing great. The limbal stem cells are taking well and today donor corneal epithelium had grown to cover most of the corneal stroma. Hopefully this is the last operation I have to do for Mr C!
Even though Mr C was unfortunate to get leukemia and then graft vs host disease, he was very lucky to have such a supportive family and sister. You really know who are the people you can count on when the going gets tough!
Update (13 August 2014)
Mr C continues to do well with clear corneas and vision of 6/12 unaided. Driving vision!







Not to forget a wonderful doc who doesn't give up. Takes a lot of strength and will from the patient too. Can imagine how heart wrenching it must have been for both when treatment fails. Well done! Always good to hear success stories.
ReplyDeleteThanks very much! Yes, it's good to keep these episodes in mind especially when things get tough again at some point in the future (as they surely will)...
Delete