What is it like having premium IOL's that correct for near vision after cataract surgery?
A very relevant question, given that nowadays there are so many lens options to choose from and also different approaches to avoid reading glasses. Here is my answer:
There are several different types of IOLs that give multifocality and good near vision as well as distance vision. I will base my answer on the most commonly used lenses-the diffractive multifocal lenses like the Alcon Restor, the Tecnis Multifocal and the Zeiss trifocal lenses.
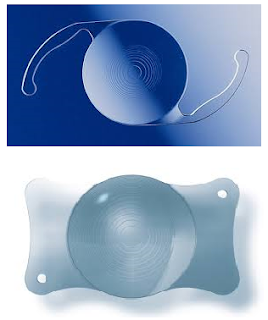 |
| The Alcon Restor lens (above), and the AT LISA tri (below) are examples of bifocal and trifocal lens implants, respectively. |
These diffractive multifocal lenses have rings etched onto either their front or back surfaces, which split/diffract incoming light rays into two foci. Some newer ones can even split the light into 3 foci. This fact gives rise to several implications.
1. Vision will be clear mainly at 2 (or sometimes 3) distances. For the older +4 Restor and the Tecnis multifocal, the near focus is at about 1 foot. So reading material has to be held quite close.
If it is held further away (say at 3 feet or so-intermediate distance), then it is not so clear anymore.
Then things much farther away, say 15-20 feet away, start to become pretty clear again. (See the figure below-only the AT LISA tri is clear at intermediate distance)
Note: This is only the case if the surgeon has been very accurate in calculating the lens power/biometry.
2. Because of the light splitting, there is a drop in contrast compared with a monofocal lens. Patients with multifocal lenses tend to be more sensitive to low light conditions-ie when it starts to get a little dark, they start to feel the drop in vision faster than patients with monofocal lenses. A person with a monofocal lens and reading glasses could read in dimmer conditions than a person with a multifocal lens.
3. The rings on the IOL give rings of light (halos) around light sources. This can be an issue when driving at night because of the halos around car headlamps. Having said this, many patients get used to the halos and do not notice it as much after a time.
 |
| Simulated halos around lights from a mutifocal lens |
The above of course does not completely apply to the Crystalens or the Oculentis MPlus. The Crystalens is an accommodative lens, which gives somewhat unpredictable results-some patients don't get any near effect at all.
The MPlus (available in Europe/Asia) has a wedged shaped section on the lens to focus for near. Point 1 above applies to this lens as well. However, although this lens does not give rings around lights, it can still cause 'halos' of a different shape-it is more like a smearing effect in one direction. Occasionally if a patient's pupil is small and not aligned with the lens, the patient may only have a far focus or a near focus and not both.
Last but not least, there is the Symfony lens which I covered in my last post. As mentioned, this is an 'in between' lens, ie in between a monofocal and a multifocal. It has no intermediate vision problems, and less halos than the usual multifocals, but does not give quite as good very near vision.
Currently, I offer patients a choice between a monofocal, an in between lens like the Symfony, and a full fledged trifocal like the AT LISA tri. I believe there is little to no benefit to be gained from using older bifocals such as the Restor and Tecnis Multifocal currently. Exactly which of those 3 choices gets implanted comes after a careful discussion with my patient regarding the pros and cons of each option. (So that we get big smiles all round afterwards!)



.jpg)



























